What is a scarless latissimus dorsi flap breast reconstruction?
|
Developed by Australian plastic surgeon, Dr Mark Lee at St John of God Hospital in Western Australia, the scarless latissimus dorsi (lat dorsi) flap is a new approach to the traditional lat dorsi breast reconstruction method that not only avoids scars to a woman’s back but also has been shown to have fewer complication rates, shorter operating time and good aesthetic outcomes. This less invasive technique may be particularly appropriate for women undergoing preventative skin and nipple sparing double mastectomies and seeking immediate reconstruction. |
Who is this technique best suited to?
As this type of procedure uses your own body tissue, a more natural looking breast can be achieved than when using implants alone. This procedure may be a good option for:
How is this surgery performed?
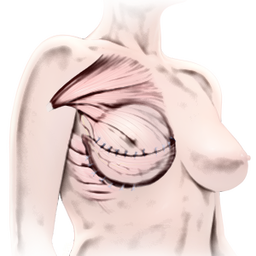
Like a traditional Latissimus Dorsi Flap reconstruction, the surgeon uses a large muscle in your back, the latissimus dorsi, to reconstruct your breast. However, rather than accessing the lat dorsi muscle through an incision on your back, the surgeon is able to access this muscle either via an incision at the outer edge of the nipple aerola, or via a submammary incision (underneath the breast area).
After your mastectomy is completed, preserving as much skin as is safe, your plastic surgeon can harvest the lat dorsi muscle, which is gently dissected and stretched across the woman’s midline and attached to her pectoral muscle in the upper part of her chest. To make the breast large enough, and achieve the desired shape and projection, implants are also needed and so the surgeon will insert a tissue expander under the muscle flap during the operation. By using implants as well as your own body tissue, a more natural looking breast can be achieved. The wound is then stitched closed.
After latissimus dorsi flap reconstruction surgery
You'll be moved to the recovery room after surgery, where hospital staff members will monitor your heart rate, body temperature, and blood pressure. If you're in pain or feel nauseated from the anesthesia, tell someone so you can be given medication.
You'll then be admitted to a hospital room. The nursing staff will check your new breast every hour to monitor the warmth, colour, tightness and blood flow. The room may be warmed or you may have a heated blanket to assist with circulation. You will have a catheter to drain urine until you are able to walk to the bathroom, usually either on the 2nd or 3rd day, and you will have several drains from the incision sites in place to remove excess blood and fluid. The drains will usually be removed 2-8 days after surgery, depending on their output.
Once you have recovered from the operation and all is progressing well with your new breast, you will be encouraged to shower and begin to move about. Nursing and physiotherapy staff will assist you in regaining mobility, and can provide advice on exercises and activities that can be done to improve your recovery and strength. You are likely to be in hospital for 4-5 days.
On leaving the hospital, your surgeon will give you specific instructions on post-operative care, including; caring for your surgical sites, medications to use, symptoms or concerns to look out for during the recovery period and when follow up is required.
How long is this operation?
A bilateral mastectomy with immediate scarless lat dorsi reconstruction takes approximately 3-4 hours. In Dr Lee’s experience, operating time was reduced by about one hour with the scarless technique when compared to the traditional lat dorsi method, due largely to the fact that the patient does not need to be turned over or repositioned during the operation. Not having to reposition the patient also reduces the risks associated with having to turn a patient while they are anaesthetised.
What is the estimated hospital stay?
The hospital stay for latissimus dorsi flap is typically 5-7 days.
Where can this surgery be performed?
This technique is very specialised, contact Dr Mark Lee in Subiaco WA.
Dr Mark Lee’s private rooms are located in the McCourt Street Medical Centre, St John of God Hospital, Subiaco. Private operating is performed at St John of God Subiaco and Hollywood Private Hospital.
Who should do this surgery for me?
This surgery is a technique that most plastic surgeons are able to perform. At the time of writing Dr Mark Lee was the only surgeon performing this technique.
What are the potential advantages of this type of surgery?
Compared to the traditional lat dorsi method, the Scarless technique:
As this type of procedure uses your own body tissue, a more natural looking breast can be achieved than when using implants alone. This procedure may be a good option for:
- Women seeking bilateral breast reconstruction
- Women who are able to have skin and nipple sparing mastectomies
- Women having prophylactic (preventative) mastectomies to reduce their cancer risk, particularly those women with the BRCA1 or BRCA2 genes.
- Women who have had radiation to the breast, are eligible to have the scarless lat dorsi procedure after a rest period for some months following radiation to allow for skin to heal. There can be further risks involved with radiated tissue such as infection and from an aesthetic point of view, damaged radiated tissue can often be difficult to expand and contour however it can still be successful in woman who are considering this surgical technique.
How is this surgery performed?
Like a traditional Latissimus Dorsi Flap reconstruction, the surgeon uses a large muscle in your back, the latissimus dorsi, to reconstruct your breast. However, rather than accessing the lat dorsi muscle through an incision on your back, the surgeon is able to access this muscle either via an incision at the outer edge of the nipple aerola, or via a submammary incision (underneath the breast area).
After your mastectomy is completed, preserving as much skin as is safe, your plastic surgeon can harvest the lat dorsi muscle, which is gently dissected and stretched across the woman’s midline and attached to her pectoral muscle in the upper part of her chest. To make the breast large enough, and achieve the desired shape and projection, implants are also needed and so the surgeon will insert a tissue expander under the muscle flap during the operation. By using implants as well as your own body tissue, a more natural looking breast can be achieved. The wound is then stitched closed.
After latissimus dorsi flap reconstruction surgery
You'll be moved to the recovery room after surgery, where hospital staff members will monitor your heart rate, body temperature, and blood pressure. If you're in pain or feel nauseated from the anesthesia, tell someone so you can be given medication.
You'll then be admitted to a hospital room. The nursing staff will check your new breast every hour to monitor the warmth, colour, tightness and blood flow. The room may be warmed or you may have a heated blanket to assist with circulation. You will have a catheter to drain urine until you are able to walk to the bathroom, usually either on the 2nd or 3rd day, and you will have several drains from the incision sites in place to remove excess blood and fluid. The drains will usually be removed 2-8 days after surgery, depending on their output.
Once you have recovered from the operation and all is progressing well with your new breast, you will be encouraged to shower and begin to move about. Nursing and physiotherapy staff will assist you in regaining mobility, and can provide advice on exercises and activities that can be done to improve your recovery and strength. You are likely to be in hospital for 4-5 days.
On leaving the hospital, your surgeon will give you specific instructions on post-operative care, including; caring for your surgical sites, medications to use, symptoms or concerns to look out for during the recovery period and when follow up is required.
How long is this operation?
A bilateral mastectomy with immediate scarless lat dorsi reconstruction takes approximately 3-4 hours. In Dr Lee’s experience, operating time was reduced by about one hour with the scarless technique when compared to the traditional lat dorsi method, due largely to the fact that the patient does not need to be turned over or repositioned during the operation. Not having to reposition the patient also reduces the risks associated with having to turn a patient while they are anaesthetised.
What is the estimated hospital stay?
The hospital stay for latissimus dorsi flap is typically 5-7 days.
Where can this surgery be performed?
This technique is very specialised, contact Dr Mark Lee in Subiaco WA.
Dr Mark Lee’s private rooms are located in the McCourt Street Medical Centre, St John of God Hospital, Subiaco. Private operating is performed at St John of God Subiaco and Hollywood Private Hospital.
Who should do this surgery for me?
This surgery is a technique that most plastic surgeons are able to perform. At the time of writing Dr Mark Lee was the only surgeon performing this technique.
What are the potential advantages of this type of surgery?
Compared to the traditional lat dorsi method, the Scarless technique:
- Avoids additional incisions and subsequent scarring on your back
- Has faster operating times, contributing to lower complication rates
- Offers reduced hospital stay – women generally go home about a day and a half earlier
- Eliminates the need to reposition the patient during surgery, reducing the risks associated with turning a patient while under anaesthetic
- Has a reduced incidence of seromas. Seromas (fluid build up) commonly occurs under the back wound with many traditional lat dorsi procedures.
What stages are involved?
What is the expected recovery time?It can take 4-6 weeks to recover from latissimus dorsi reconstruction surgery and to resume normal activities.
|
"After speaking with 2 plastic surgeons I chose the double Scarless Lat Dorsi as I didn't have enough tummy fat for DIEP and it made sense to not have 2 extra wounds to heal on my back and extra support to hold the implants in place. I also liked the idea it cut down the operation time by about an hour. I had viewed implant only pics at the breast clinic but preferred the finished look of Lat Dorsi. |
What are the risks?
Like all surgery, latissimus dorsi flap surgery has some risks. Many of the risks associated with latissimus dorsi flap surgery are the same as the risks for mastectomy. If you've had an implant inserted along with latissimus dorsi reconstruction, there are also risks related to implant reconstruction. However, there are some risks that are unique to latissimus dorsi flap reconstruction.
Tissue breakdown
In rare instances, the tissue moved from your back to your breast area won't get enough circulation and some of the tissue might die. Doctors call this tissue breakdown “necrosis.” Some symptoms of tissue necrosis include the skin turning dark blue or black, a cold or cool-to-the-touch feeling in the tissue, and even the eventual development of open wounds. You also may run a fever or feel sick if these symptoms are not addressed immediately. If a small area of necrosis is found, your surgeon can trim away the dead tissue. This is done in the operating room under general anesthesia or occasionally in a minor procedure setting. If most or all of the flap tissue develops necrosis, your doctor may call this a “complete flap failure,” which means the entire flap would need to be removed and replaced. Sometimes the flap can be replaced within a short timeframe, but in most cases the surgical team will remove all the dead tissue and allow the area to heal before identifying a new donor site to create a new flap.
Lumps in the reconstructed breast
If the blood supply to some of the fat used to rebuild your breast is cut off, the fat may be replaced by firm scar tissue that will feel like a lump. This is called fat necrosis. These fat necrosis lumps may or may not go away on their own. They also might cause you some discomfort. If the fat necrosis lumps don't go away on their own, it's best to have your surgeon remove them. After having mastectomy and reconstruction, it can be a little scary to find another lump in your rebuilt breast. Having them removed can give you greater peace of mind, as well as ease any discomfort you might have.
Muscle weakness
In some cases, you may have some weakness in your back, shoulder, or arm after latissimus dorsi flap breast reconstruction because some of your back muscle has been moved to your chest. You may have partial loss of strength or function that makes it hard to lift things and twist. This can affect your ability to perform certain swimming, golf, or tennis stokes, or turn and manipulate objects. If you have muscle weakness that is problematic and persistent, talk to your doctor to see if you can work with a physical therapist on these issues. Also, ask about exercises you can do to help strengthen the area.
Fluid under the back wound (seroma)
This is the most common problem which occurs with this type of surgery. Seromas usually get better with time and as the body heals, but sometimes they need to be drained by the surgeon, or another skilled health professional.
Tissue breakdown
In rare instances, the tissue moved from your back to your breast area won't get enough circulation and some of the tissue might die. Doctors call this tissue breakdown “necrosis.” Some symptoms of tissue necrosis include the skin turning dark blue or black, a cold or cool-to-the-touch feeling in the tissue, and even the eventual development of open wounds. You also may run a fever or feel sick if these symptoms are not addressed immediately. If a small area of necrosis is found, your surgeon can trim away the dead tissue. This is done in the operating room under general anesthesia or occasionally in a minor procedure setting. If most or all of the flap tissue develops necrosis, your doctor may call this a “complete flap failure,” which means the entire flap would need to be removed and replaced. Sometimes the flap can be replaced within a short timeframe, but in most cases the surgical team will remove all the dead tissue and allow the area to heal before identifying a new donor site to create a new flap.
Lumps in the reconstructed breast
If the blood supply to some of the fat used to rebuild your breast is cut off, the fat may be replaced by firm scar tissue that will feel like a lump. This is called fat necrosis. These fat necrosis lumps may or may not go away on their own. They also might cause you some discomfort. If the fat necrosis lumps don't go away on their own, it's best to have your surgeon remove them. After having mastectomy and reconstruction, it can be a little scary to find another lump in your rebuilt breast. Having them removed can give you greater peace of mind, as well as ease any discomfort you might have.
Muscle weakness
In some cases, you may have some weakness in your back, shoulder, or arm after latissimus dorsi flap breast reconstruction because some of your back muscle has been moved to your chest. You may have partial loss of strength or function that makes it hard to lift things and twist. This can affect your ability to perform certain swimming, golf, or tennis stokes, or turn and manipulate objects. If you have muscle weakness that is problematic and persistent, talk to your doctor to see if you can work with a physical therapist on these issues. Also, ask about exercises you can do to help strengthen the area.
Fluid under the back wound (seroma)
This is the most common problem which occurs with this type of surgery. Seromas usually get better with time and as the body heals, but sometimes they need to be drained by the surgeon, or another skilled health professional.
What are the costs?
Private hospital costs
Most surgeons charge AMA rates, (ie rates that the Australian Medical Association recommends) plus anaesthetic and theatre costs set by your surgical team and selected hospital. Additional costs may include a hospital excess, tests, post-surgery garments and medications.
Out of pocket expenses can vary widely and it is important that you request a written quote from your surgeon and anaesthetist before committing to any surgery. Breast reconstruction surgery is considered a reconstructive, not a cosmetic procedure, and is generally covered by private health insurance. If you have private health insurance cover you will need to review your policy carefully with your provider to determine exactly what is covered before proceeding.
Most surgeons charge AMA rates, (ie rates that the Australian Medical Association recommends) plus anaesthetic and theatre costs set by your surgical team and selected hospital. Additional costs may include a hospital excess, tests, post-surgery garments and medications.
Out of pocket expenses can vary widely and it is important that you request a written quote from your surgeon and anaesthetist before committing to any surgery. Breast reconstruction surgery is considered a reconstructive, not a cosmetic procedure, and is generally covered by private health insurance. If you have private health insurance cover you will need to review your policy carefully with your provider to determine exactly what is covered before proceeding.
Preparation advice
|
Recovery adviceIt can take about 4-6 weeks to recover from latissimus dorsi reconstruction surgery. A support bra may be worn to help reduce swelling and support the reconstructed breast. You may be prescribed painkillers, antibiotics and anti-inflammatory drugs when you are first discharged from hospital. It is vital to use these as prescribed to successfully manage any pain and to reduce the risk of infection. Post-operative recovery can take longer if complications occur, so it is important to get adequate rest, make sure you follow your surgeon’s directions and exercise within the limits of comfort – if you feel any pain or pulling, especially around the wound sites, stop. Follow your doctor's advice on when to start stretching exercises and your normal activities. You usually have to avoid lifting anything heavy, strenuous sports, and sexual activity for about 4 weeks after latissimus dorsi flap reconstruction. It’s worth having a short course of physical therapy with a qualified breast cancer physical therapist to strengthen and maintain range of motion in your shoulder. Ask your doctor for recommendations. It can take up to twelve months to completely heal and for scars to fade and for you to get a good indication of how your new breasts will settle into your body. If you were not able to have a nipple sparing mastectomy, you may like to consider the finishing touch of reconstructed nipples or 3D nipple tattoos. |
Reviewed by:
Dr Mark Lee
MBBS FRACS (Plastic Surgery)
Reference sources:
www.markleeplasticsurgeon.com.au
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4174076/
http://www.plasticsurgery.org/news/2014/scarless-flap-provides-new-alternative-for-breast-reconstruction.html
Dr Mark Lee
MBBS FRACS (Plastic Surgery)
Reference sources:
www.markleeplasticsurgeon.com.au
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4174076/
http://www.plasticsurgery.org/news/2014/scarless-flap-provides-new-alternative-for-breast-reconstruction.html